PRP Activation Activation of PRP was performed by adding 10% of CaCl 2 (final concentration 22.8 mM), 10% of autologous thrombin, 10% of a mixture of CaCl 2 + thrombin, and 10% of collagen type I (final concentration 4 μ g) (Mascia Brunelli SpA, Milan). PRP without activation and PPP were used as control.
How do you activate PRP with PPP?
Activation is a crucial step in effective platelet rich plasma (PRP) protocols. Activation occurs after centrifugation and initiates the platelet degranulation process. Platelet degranulation releases bioactive proteins known as growth factors which increase cell mitosis, angiogenesis, chondrogenesis, and chemotaxis. Essentially, activated platelets initiate the healing cascade in …
How does platelet activation affect PRP releasate?
Jul 02, 2021 · PRP treatment has shown benefit in many aspects of medicine, including hair loss, skin rejuvenation, scar treatments, arthritis and joint inflammation. In order to get the best PRP treatment, you should consider the type of preparation system, making sure that it is safe and effective. As well, you should ask about the experience and training ...
How to prepare platelet rich plasma (PRP)?
However, I stopped activation of PRP prior to injection for the last year, with exactly the same clinical success. It is thought that exposed collagen in damaged joints will activate the PRP.
What happens during PRP treatment?
unactivated PRP may result in a more normal physiologic activation by the injected tissue. To avoid unintentional activation ofplatelets , most protocols use large bore needles (>22) to draw the blood and re-inject PRP.
When should I activate PRP?
Activation is a crucial step in effective platelet rich plasma (PRP) protocols. Activation occurs after centrifugation and initiates the platelet degranulation process. Platelet degranulation releases bioactive proteins known as growth factors which increase cell mitosis, angiogenesis, chondrogenesis, and chemotaxis.Aug 10, 2020
How can I make PRP more effective?
How You Can Improve Your PRP OutcomeHigh Intensity Cardio Exercise. ... Eat a Diet Rich in Green Leafy Vegetables. ... Don't Smoke, Drink or do Drugs. ... Increase B-Vitamins and Hydrate. ... Avoid Non-Steroidal Anti-Inflammatory Drugs (NSaid) ... Follow Your Post-Procedure Routine.
What stimulates PRP?
During the treatment, a technician draws your blood and spins it in a centrifuge to separate out the platelets and plasma. Doctors then inject the plasma, which helps repair blood vessels, promote cell growth and wound healing, and stimulate collagen production.Dec 22, 2020
How long does PRP take to activate?
Depending on your condition, you should see results between 2-6 weeks after receiving a PRP injection. Mild injuries or chronic pain cases typically see results within the first two weeks, while more serious injuries won't be able to appreciate the healing until around a month has passed.
How do you spin blood for PRP?
PRP method Centrifuge the blood using a 'soft' spin. Transfer the supernatant plasma containing platelets into another sterile tube (without anticoagulant). Centrifuge tube at a higher speed (a hard spin) to obtain a platelet concentrate. The lower 1/3rd is PRP and upper 2/3rd is platelet-poor plasma (PPP).
What rpm do you spin PRP?
The PRP centrifuge RPM and time can vary between genders – such as 3,000 RPM at 3 minutes for women, 3,000 RPM at 4 minutes for men. Certain patients—like those who are taking drugs like aspirin or with conditions like anemia—might need a centrifuge of 2,200 RPM at 4 minutes instead.Sep 23, 2020
Is minoxidil necessary after PRP?
The first 12 months of treatment is very important and Minoxidil should be continued twice daily or else the expected benefits may not happen. It is a good maintenance drug with minimal side effects.Nov 5, 2016
How do you inject PRP into your face?
The process begins by drawing a couple of vials of blood from the arm of the patient. The blood is centrifuged to separate the platelets from the rest of the blood. A local anesthetic is applied to the face, and the platelets are shot into the face via mini injection holes.Oct 24, 2017
Is PRP halal?
Therefore, the authors state that the law of the use of PRP treatment for the purpose of treating injuries is permissible. This is because it is embodied in medicine that is classified as an emergency.Jun 11, 2021
How deep do you inject PRP?
Interfollicular A-PRP injections (0.2 mL x cm2) were performed by controlled and mechanical injections scheduled at a depth of 5 mm using a medical injector gun. Treatment sessions were performed with a 30-day interval. For each patient, three treatment sessions were performed.Jan 27, 2018
How long does platelet-rich plasma last?
Platelet-rich plasma lasts anywhere from six and nine months, during which time it will continue to aid in healing the soft-tissue injury.
What should I do before PRP treatment?
Pre-Procedure Don'tsDon't use any hair products like hairspray or gel for at least three days prior to your PRP injections. This can negatively affect you later in terms of side effects.Don't smoke or drink heavily beforehand, if at all.
How to prepare PRP?
There are many ways of preparing PRP. It can be prepared by the PRP method or by the buffy-coat method. In the PRP method, an initial centrifugation to separate red blood cells (RBC) is followed by a second centrifugation to concentrate platelets, which are suspended in the smallest final plasma volume.
What is PRP dermatology?
The utility of platelet-rich plasma (PRP) has spanned various fields of dermatology from chronic ulcer management to trichology and aesthetics, due to its role in wound healing. Though PRP is being used over a long time, there is still confusion over proper terminology to define, classify and describe the different variations ...
Does PRP affect platelet aggregation?
In several species that alterations in the pH and extracellular iCa concentration of PRP can affect platelet aggregation in vitro, with aggregation typically impaired at acidic pH and lower extracellular iCa concentrations.[39,40] Alternatively citrate phosphate dextrose-adenine) can be used.
What is platelet rich plasma?
Platelet-Rich Plasma (PRP) is a low-cost procedure to deliver high concentrations of autologous growth factors (GFs). Platelet activation is a crucial step that might influence the availability of bioactive molecules and therefore tissue healing. Activation of PRP from ten voluntary healthy males was performed by adding 10% of CaCl 2, 10% of autologous thrombin, 10% of a mixture of CaCl 2 + thrombin, and 10% of collagen type I. Blood derivatives were incubated for 15 and 30 minutes and 1, 2, and 24 hours and samples were evaluated for the release of VEGF, TGF- β 1, PDGF-AB, IL-1 β, and TNF- α. PRP activated with CaCl 2, thrombin, and CaCl 2 /thrombin formed clots detected from the 15-minute evaluation, whereas in collagen-type-I-activated samples no clot formation was noticed. Collagen type I produced an overall lower GF release. Thrombin, CaCl 2 /thrombin, and collagen type I activated PRPs showed an immediate release of PDGF and TGF- that remained stable over time, whereas VEGF showed an increasing trend from 15 minutes up to 24 hours. CaCl 2 induced a progressive release of GFs from 15 minutes and increasing up to 24 hours. The method chosen to activate PRP influences both its physical form and the releasate in terms of GF amount and release kinetic.
What is the Kolmogorov Smirnov test?
The Kolmogorov Smirnov test was performed to test normality of continuous variables. The area under the curve of release at every time of measurement was calculated for each activation method to quantify the amount and kinetics of the released molecules. The Repeated Measures General Linear Model (GLM) with Sidak test for multiple comparisons was performed to assess the differences at different follow-up times in each activation method. The Repeated Measures GLM was also used to assess the influence of the different activation methods.
Is tissue repair a slow process?
1. Introduction. Tissue repair in musculoskeletal injuries is often a slow and sometimes incomplete process, with patient suffering pain and limited function, and therefore it is accompanied by high costs to society, in terms of both money spent on healthcare and also loss of work.
There are two different types of platelet activation
Endogenous. This activation occurs naturally. It is also known as “physiological activation”, and it happens as the platelets react to the collagen fibers inside the body. Some authors recommend applying the platelets directly and letting them act on their own.
How to choose the appropriate activation method?
Different research studies have determined that CaCl2 10% and CG 10% are the easier ones to obtain, regarding availability and cost.
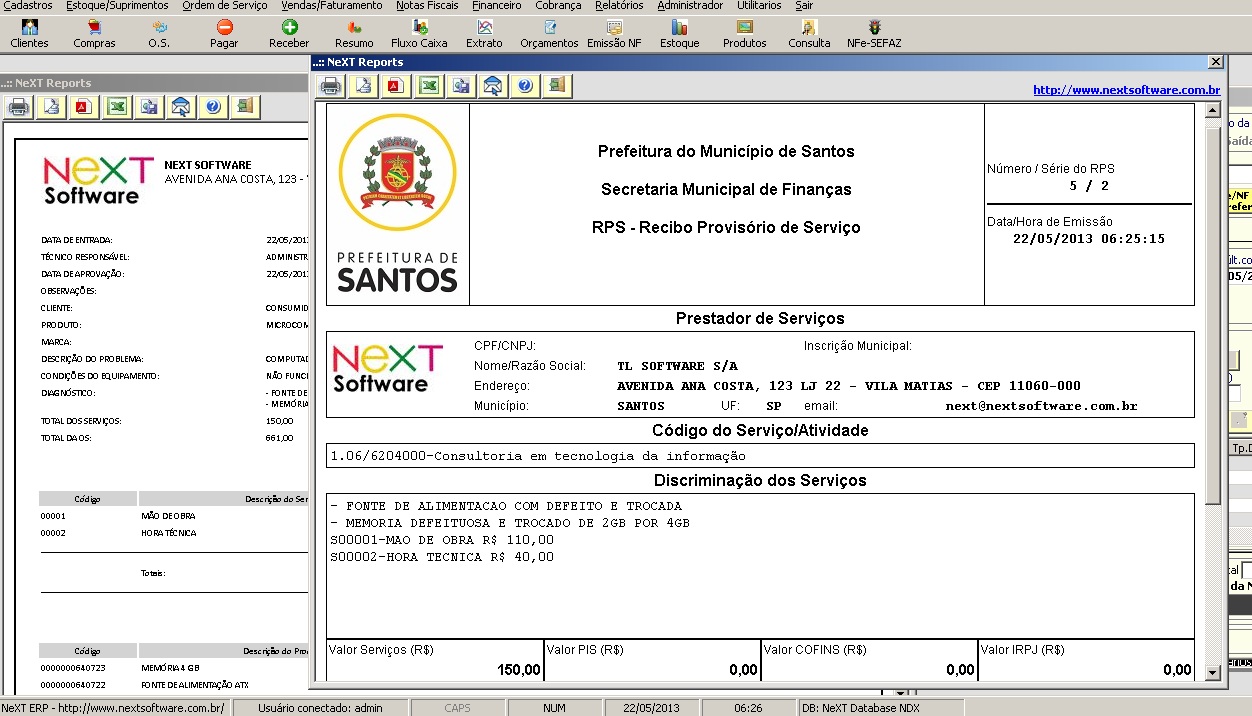
Research Study in Brazil
A research study made in Brazil in 2012 by Zandim et al., evaluated the effect of BT, CaCl2, and physiological activation in horse platelets, by analyzing the platelet morphology and activation state after the activation process.
Other Studies Done
Another study made in feline platelets by Silva et al. was published in BMC Veterinary Research also in 2012, and compared BT against CG for platelet activation. The results measured platelet efficiency, and showed 61.36% efficiency for CG activated PRP, and 65.64% for BT activation.
Who should perform PRP injections?
PRP injections should be performed by allopathic or osteopathic physicians with a valid license to practice medicine and surgery in the State in which they practice. Successfully and safely performing PRP procedures requires knowledge of the diagnosis, standard treatments, benefits, risks, contraindications, methods of preparation and delivering it to the appropriate patient in the appropriate situation.
When was PRP first used?
First promoted by M. Ferrari in 1987 (1) as an autologous transfusion component after an open heart operation to avoid homologous blood product transfusion, there are now over 5200 entries in the NCBI for PRP ranging in fields from orthopedics, sports medicine, dentistry, otolaryngology, neurosurgery, ophthalmology, urology, wound healing, cosmetic, cardiothoracic and maxillofacial surgery.
How long does it take for PRP to heal?
PRP is generally considered an elective treatment for subacute and chronic conditions. Generally, healing slows or stops 6-12 weeks after an acute injury. If a patient has had no improvement for over six weeks, it is possible their healing phase has arrested. In overuse or repetitive conditions, it can be more challenging to isolate the transition from an acute phase.
Is tendinopathy a degenerative condition?
Tendinopathy refers to a degenerative condition of tendons marked by the chronic loss of collagen, tissue integrity, stability and strength. Tendinopathy is not an inflammatory condition, as histologic specimens lack inflammatory cells (11). Causes are multifactorial, but natural aging, injury, repetitive stress, neural, vascular and hormonal inputs all likely contribute. Whereas tendinopathy is nearly ubiquitous as we age, pain and dysfunction generally occur only when sufficient stresses are applied to the degenerated tendon.
Does PRP have a higher platelet concentration than baseline?
By definition, PRP must contain a higher concentration of platelets than baseline, however an increase in platelets is a very gross description of PRP and does not accurately describe the variability among different types of PRP. There are several parameters that need to be taken into account when considering PRP, including: platelet concentration above baseline, whether or not leucocytes are included, whether or not the PRP has been anticoagulated and whether it requires exogenous activation.
What is centrifugation in PRP?
Centrifugation is a technology that separates the blood cells from the plasma liquid. It is the first step done in PRP to harvest autologous platelets for the treatment injection. To do this, a clinician must carefully use a syringe to draw a blood sample from the patient’s arm.
What is platelet rich plasma?
Platelet rich plasma (PRP) therapy is a form of regenerative medicine that utilizes autologous platelets for treatment of various medical and aesthetic issues. During PRP, a patient receives injections of their own platelet concentrate to stimulate the body’s natural healing properties.
How to separate plasma from WBC?
1. Gel Separator . This is one of the simplest ways to separate the plasma from the RBC and WBC. With this system, a tube will be filled with a gel substance that will isolate the platelet from the white blood cells and red blood cells through the process of osmosis.
Where are stem cells found?
These stem cells are abundant in the bone marrow and are capable of mutating into red blood cells, white blood cells, and platelets. The doctors who study blood have discovered many uses to this liquid and one of these advancements is the platelet-rich plasma therapy.
What are the components of blood?
To better understand the process of PRP preparation, it’s important to first know the four main components of the human blood and its important functions: Red blood cell- Also known as RBCs or erythrocytes, they account for almost 45% of the fluid of blood.
How long does it take for a centrifuge to rotate blood?
Most centrifuge devices rotate the blood for an average of 10 minutes. There’s a study that shows the correlation of time with the final composition of the PRP sample. In the trial, they took blood samples and initiated their first spin at a low setting for 6 and 10 min.
Does PRP help with hair loss?
Aesthetics clinics also offer PRP for hair loss problems among women and androgenic alopecia in men. Platelet-rich plasma therapy is injected into the scalp to improve overall scalp health and stimulates healing of hair follicle tissues which serve as the root of the hairs.
How long do platelets last?
Platelet concentration in blood is approximately 300,000/ul, and they normally have a half-life of 4 days. They are formed from committed giant stem cells called megakaryocytes as they pinch off bits of their cytoplasm and extrude them into the blood circulation. Platelets have microtubules around their periphery and an extensively invaginated membrane in contact with extracellular fluid.
Why are clotting times longer in vitro?
The longer clotting times obtained in vitro could be an indication that the concentrations of clotting precursors and enzymes may be relatively low in serum and it takes time for the reactions to develop . However, once activation was initiated subsequent clotting proceeded rapidly. This is consistent with the autocrine/ paracrine nature of intercellular communication via chemical mediators during platelet activation. Anitua et al1 states that the administration of activated platelets in fibrin clot or fibrin glue provides an adhesive support that can confine secretion to a chosen site, and the presentation of growth factors attached to platelets and/or fibrin may result in enhanced activity over recombinant proteins. Extended in vitro activation times could be advantageous when autogenous bone, allografts and xenografts are to be mixed with PRP before placement in situ for ridge augmentation grafts, ridge maintenance grafts, sinus elevation grafts, repair of schneiderian membrane as well as rapid soft tissue healing and maturation.
Abstract
- Platelet-Rich Plasma (PRP) is a low-cost procedure to deliver high concentrations of autologous growth factors (GFs). Platelet activation is a crucial step that might influence the availability of bioactive molecules and therefore tissue healing. Activation of PRP from ten voluntary healthy males was performed by adding 10% of CaCl2, 10% of autologous thrombin, 10% of a mixture of …
Introduction
- Tissue repair in musculoskeletal injuries is often a slow and sometimes incomplete process, with patient suffering pain and limited function, and therefore it is accompanied by high costs to society, in terms of both money spent on healthcare and also loss of work. Thus, many efforts have been made in order to investigate new approaches to increase the regenerative potential a…
Materials and Methods
- This study was approved by the local Ethics Committee and the Institutional Review Board, and each donor signed an informed written consent. PRP, Platelet-Poor Plasma (PPP), and autologous thrombin were obtained from ten voluntary healthy men (mean age ± SD: years) who underwent a blood sample collection of 150 mL. Subjects did not present with systemic disorders, smoking h…
Results
- The median number of platelets per cubic millimeter was , , and for PB, PP, and PRP, respectively. The median concentration of white blood cells per cubic millimeter was , , and for PB, PP, and PRP, respectively. CaCl2, thrombin, CaCL2/thrombin, and collagen type I induced a different platelet aggregation. In particular, PRP activated with CaCl2, thrombin, and CaCL2/thrombin for…
Discussion
- The main finding of our study is that the activation modality influences PRP clot formation, leading to differences in terms of both amount and release kinetics of platelet-derived GFs. The most commonly used activation methods in the current clinical practice [14 1. D. Fufa, B. Shealy, M. Jacobson, S. Kevy, and M. M. Murray, “Activation of platelet-rich plasma using soluble type I c…
Competing Interests
- Giuseppe Filardo is consultant and receives institutional support from Finceramica Faenza SpA (Italy), Fidia Farmaceutici SpA (Italy), and CartiHeal (2009) Ltd. (Israel). He is a consultant for EON Medica SRL (Italy). He receives institutional support from IGEA Clinical Biophysics (Italy), BIOMET (USA), and Kensey Nash (USA). Elizaveta Kon is a consultant for CartiHeal (2009) Ltd. (Israel) an…
Acknowledgments
- The authors thank Dr. Elettra Pignotti for statistical assistance and Mr. Keith Smith for English editing, Rizzoli Orthopaedic Institute, Bologna, Italy. This work was supported by grants from “” funds, Italian Ministry of Health (Project RF-2009, Grant no. 1498841), and Emilia-Romagna Region (Region-University Program 2010–2012: Regenerative Medicine of Cartilage and Bone).
There Are Two Different Types of Platelet Activation
- Endogenous. This activation occurs naturally. It is also known as “physiological activation”, and it happens as the platelets react to the collagen fibers inside the body. Some authors recommend ap...
- Exogenous. This type of activation is pharmacologically induced before applying the PRP onto the patient. The most commonly used products for veterinary use are Calcium Gluconate at 1…
- Endogenous. This activation occurs naturally. It is also known as “physiological activation”, and it happens as the platelets react to the collagen fibers inside the body. Some authors recommend ap...
- Exogenous. This type of activation is pharmacologically induced before applying the PRP onto the patient. The most commonly used products for veterinary use are Calcium Gluconate at 10% (CG), Calci...
How to Choose The Appropriate Activation Method?
- Different research studies have determined that CaCl2 10% and CG 10% are the easier ones to obtain, regarding availability and cost. When using CaCl2 10%, the dilution should be 0.1 cc of CaCl2 for every 0.9 cc of PRP, so that neutralization of the anticoagulant effect of the citrate can be achieved. In the case of CG 10%, the dilution should be 0.3 cc of CG for every 0.7 cc of PRP. T…
Research Study in Brazil
- A research study made in Brazil in 2012 by Zandim et al., evaluated the effect of BT, CaCl2, and physiological activation in horse platelets, by analyzing the platelet morphology and activation state after the activation process. In this study, BT showed not suitable for equine platelet activation, since the platelets where seen as irregularly shaped, as well ruptured granules both in…
Other Studies Done
- Another study made in feline platelets by Silva et al. was published in BMC Veterinary Research also in 2012, and compared BT against CG for platelet activation. The results measured platelet efficiency, and showed 61.36% efficiency for CG activated PRP, and 65.64% for BT activation. The author’s conclusion was that both activators provide a very useful platelet concentration and effi…
Popular Posts:
- 1. how to activate tech armor warranty
- 2. how to activate vodafone data pack
- 3. archeage how to activate fish hole
- 4. how to activate bixby voice on s9
- 5. how to activate international roaming on my jio app
- 6. how can i re-activate a t-mobile hotspot
- 7. how to activate new phone number on page plus
- 8. how to activate product key office 2016
- 9. how to activate facebook dating in nigeria
- 10. where to go to activate windows